HPV and the LGBTIQ+ Communities
The reality is, anyone in the LGBTIQ+ Communities can be exposed to HPV and need HPV related healthcare.
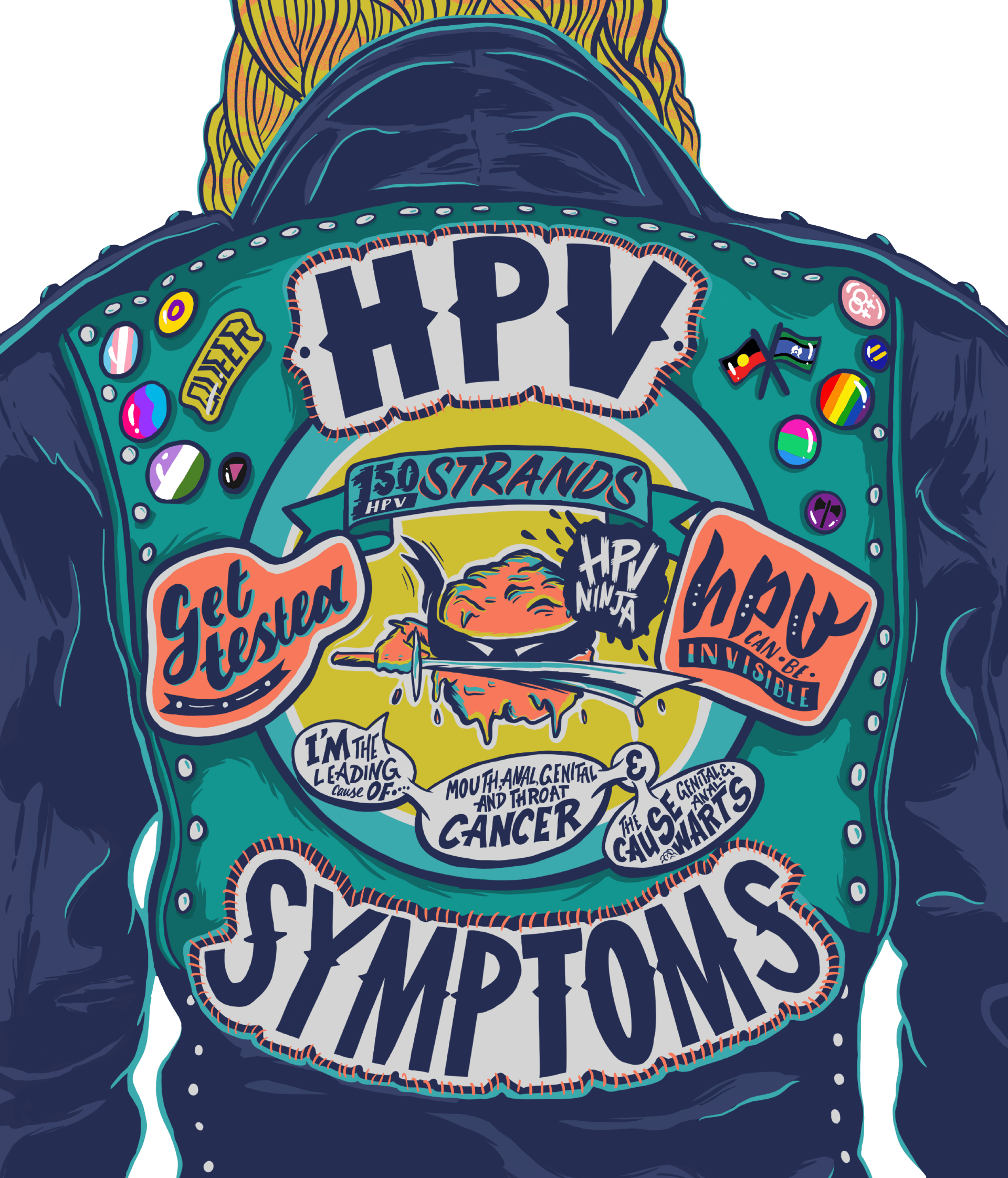
HPV is the Human Papillomavirus. It is a highly transmissible virus, shared via skin-to-skin contact. There are 150+ strands of the HPV virus.
Anyone, having any kind of sex with other people, regardless of bodies, genders or sexualities, can have and transmit HPV.
If you get HPV, usually your own immune system will fight it off, but when your body can't fight off HPV, it can lead to:
- Genital or anal warts,
- Genital, anal, mouth or throat cancers, or,
- Cervical cancer.
What is HPV?
Signs, Symptoms and Treatment
It can be tricky to know if you have HPV.
HPV can only be detected from a cervical screening test, so if you don’t have a cervix you can’t actually be tested for HPV.
Many people will have HPV but never know.
Many people who are tested and diagnosed with HPV are unsure when they came into contact with it, especially if they haven’t been sexually active for a long time or are in monogamous relationships.
This is common and isn’t something to worry about, it is very likely you came into contact with HPV a long time ago and are only seeing symptoms now, or only now returning an abnormal cervical screening result.
As not everyone can be tested for HPV, it
is important to look out for signs and symptoms.
HPV symptoms can vary depending on which strand of HPV you have.
There are 150+ strands, and some strands of HPV lead to warts, and other strands to cancers.
HPV symptoms may not appear for weeks, months or years after you first come into contact with the virus.
Warts
Gential or anal warts look like teeny, tiny cauliflowers. They can be white or skin coloured.
Warts can only be removed by a healthcare professional. If you have genital or anal warts, your GP will talk through treatment options with you.
However, treatment for genital or anal warts is not a cure for HPV. Treating warts only removes the warts, you will still have HPV, but, it’s likely your immune system will keep fighting until you no longer have HPV. This can take time (sometimes this can take years), so it’s important to keep checking your body for any changes or return of warts, and continue practicing safer sex.
QUEER ALERT
Over the counter creams/treatments for foot or hand warts do not work on genital or anal warts.
Genital, anal, mouth or throat cancer
HPV is the leading cause of genital, anal, mouth and throat cancers. It’s actually more common to develop mouth or throat cancer from HPV than it is from smoking.
A HPV related cancer may be hard to spot, so keep an eye out for any changes in your body. If anything seems off or different to your usual, head to your GP straight away to investigate.
Cervical Cancer
HPV is the leading cause of cervical cancer.
Cervical Cancer is only visible and detectable by a Cervical Screening Test. Anyone with a cervix, regardless of your body, gender or sexuality, needs a cervical screening test.
If your Cervical Screening Test returns a positive result for HPV infection, your doctor will advise on next steps according to your specific circumstances.
You know your body better than anyone else. If you notice any changes in your body, talk to your GP or healthcare provider immediately.
Prevention and Testing Options
Regardless of our bodies, genders or sexualities, we can all reduce our risk of HPV.
Some simple measures include:
- Safer sex,
- Checking your body for signs and symptoms,
- Regular sexual health check-ups,
- Getting the Gardasil vaccines, and,
- Getting cervical screening tests if you have a cervix.
1. Safer Sex
As HPV is transmitted through skin to skin contact, using protective barriers like condoms, gloves and dental dams reduces our risk of contracting HPV.
2. Check for signs and symptoms
Look out for the presence of genital or anal warts. Pay attention to any changes, growths, pain or discomfort in your mouth or throat.
Keep across any changes, growths, pain or discomfort to your genitals, anus or rectum. See your GP immediately if you notice any changes. It could be HPV related.
3. Sexual Health Check-ups
Regular or yearly sexual health check-ups are a great way to see if you are showing any signs or symptoms of HPV.
In particular you want your doctor to check for any abnormalities to your mouth, throat, genitals and anus.
Even though the only HPV test we currently have is a cervical screening test, there are other physical examinations your doctor can perform. For example, a rectal examination (ie a finger up the bum) is an easy way for your doctor to feel for any HPV related lesions.
4. Cervical Screening Tests
Anyone with a cervix, regardless of your body, gender or sexuality, needs a cervical screening test.
Cervical screening tests are available for anyone with a cervix who is over 25yrs of age or anyone who is already sexually active.
A cervical screening test should be performed every 5 years.
All cervical screening participants now have the choice to self-collect their own Cervical Screening Test sample. A self-collected sample is taken from the vagina so you don’t need to worry about reaching the cervix or ‘getting the right spot’. All you need to do is insert a swab a few centimetres into your vagina and rotate it for 20 to 30 seconds. You will be given a private space, such as a bathroom, to collect your sample.
Evidence shows a Cervical Screening Test using a self-collected sample from your vagina is just as accurate at detecting HPV as a clinician-collected sample taken from the cervix during a speculum examination.
QUEER ALERT
Why is a cervical screening test done every 5 years when a pap smear was required every 2 years?
Simply put, a pap smear looked for cancerous cells on the cervix while a cervical screening test looks for the presence of HPV. By testing for HPV we are monitoring and treating HPV early before it becomes cancerous, this makes a cervical screening test more efficient than a pap smear and therefore not required as often. The introduction of the Gardasil vaccine also reduces the risk of HPV developing into cancers and further supports a 5 year testing cycle.
5. Gardasil Vaccine
Gardasil is a highly effective vaccine that protects against the most common strands of HPV that cause both warts and cancers.
The Gardasil vaccine protects against approximately:
● 90% of cervical cancers,
● 90% of genital warts
● 91% of anal cancer,
● 80% of vulvar and vaginal cancers,
● 63% of penile cancers and
● 89% of throat cancers.
Anyone, of any age, gender, body or sexuality can access the Gardasil vaccines. Chat to your doctor about costs and the benefits of the vaccine for your unique circumstances. For example, it is recommended that people who are living with HIV should have the vaccine.
QUEER ALERT
The Gardasil vaccine is now available to all students aged 12-13 years as part of the school-based National HPV Vaccination Program.
Tips for Accessing Healthcare
Watch the videos below to learn valuable tips on how to get the most from your doctor visits and how to make these visits a less stressful experience.
Ask a Doctor:
All your HPV questions answered
Step inside a LGBTIQ+ friendly GP office to get all your questions answered around HPV: what is is, how to get a test as a LGBTIQ+ person, screening options, treatment, prevention, and more.
Brisbane GP Dr Fiona Bisshop has been working in LGBT health and HIV medicine since 2001, and has an active interest in research. She is an S100 prescriber, and offers holistic HIV management, PrEP and advice on all sexual health matters.